Parts
The Common Vein Copyright 2008
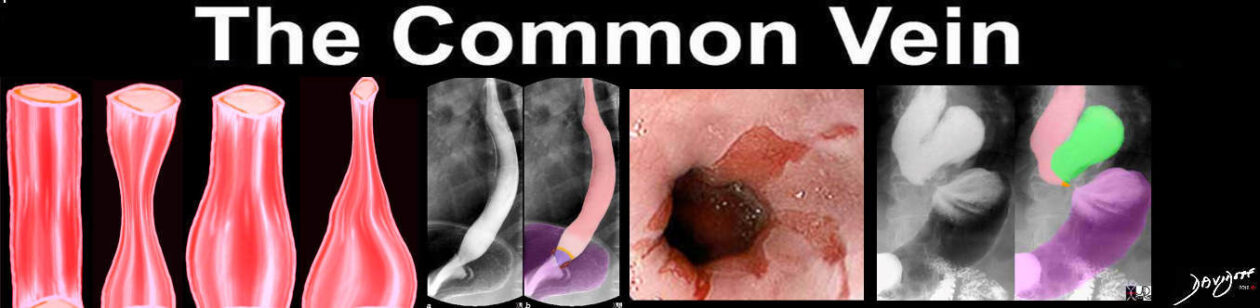
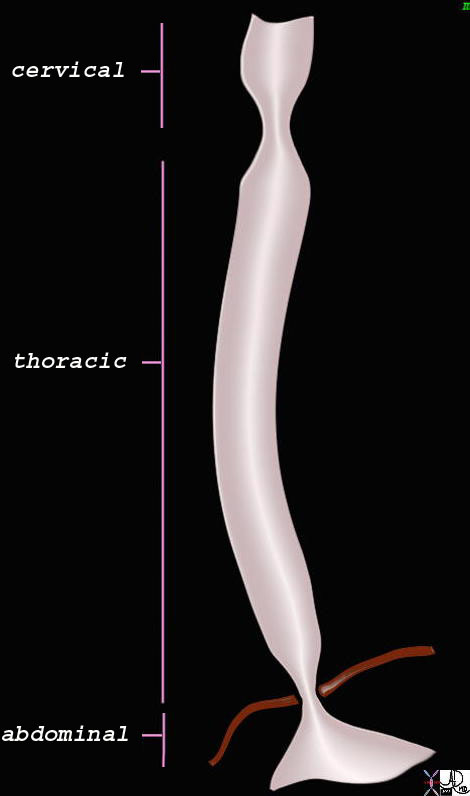
The esophagus can be divided into 3 main sections: the cervical, thoracic and abdominal portions.
The upper esophageal sphincter at the junction of the pharynx and the esophagus is called the cricopharyngeal muscle. The lower sphincter between the esophagus and the stomach is called the lower esophageal or cardiac sphincter.
keywords
esophagus normal motility contraction wave peristalsis primary stripping wave physiology function receptive relaxation upper esophageal sphincter lower esophageal sphincter LES UES esophageal body pharynx
Courtesy Ashley Davidoff MD TheCommonVein.net
73368b07b
The cervical esophagus is the first part. It starts around C5 (5th cervical vertebra), or approximately 15cm from the incisors. The trachea runs just anterior to the cervical esophagus. Several nerve fibers, such as the recurrent laryngeal nerve course between these structures. The thyroid can overlap the upper portion of the esophagus.
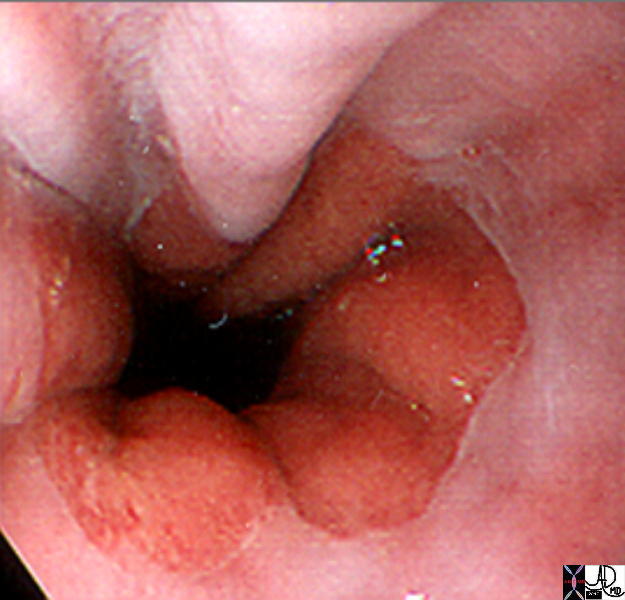
Upper Esophageal Sphincter
Upper Esophageal Sphincter
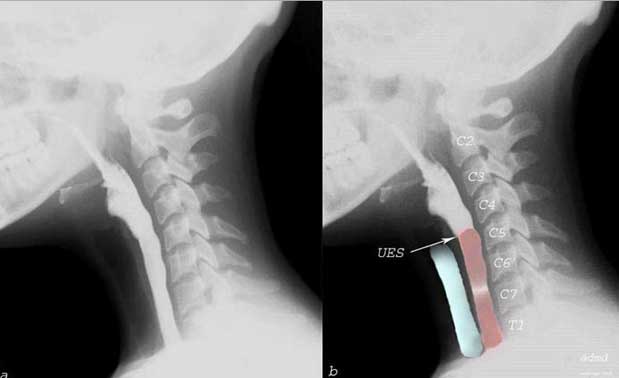
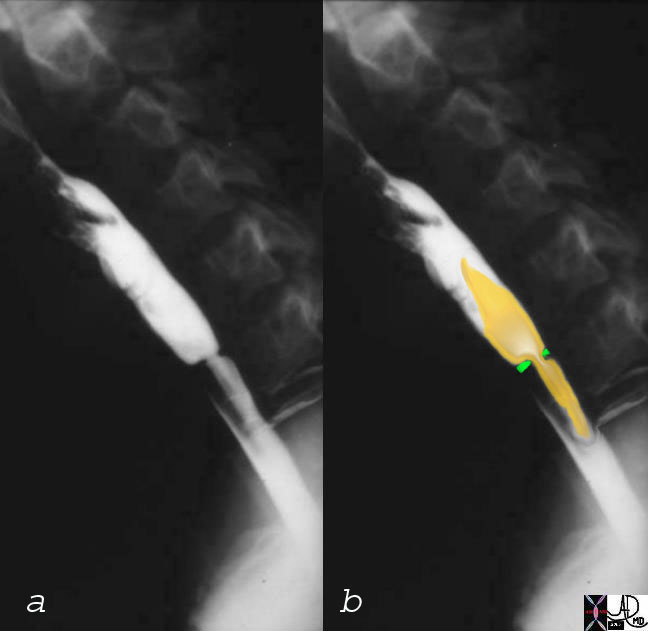
The barium swallow shows contrast moving from the back of the mouth into the pharynx into an open upper esophageal sphincter (UES), as it enters the cervical esophagus (pink) at C5. The trachea is overlaid in blue and lies anterior to the esophagus.
Ashley Davidoff, M.D. TheCommonVein.net 76204c
Thoracic Esophagus

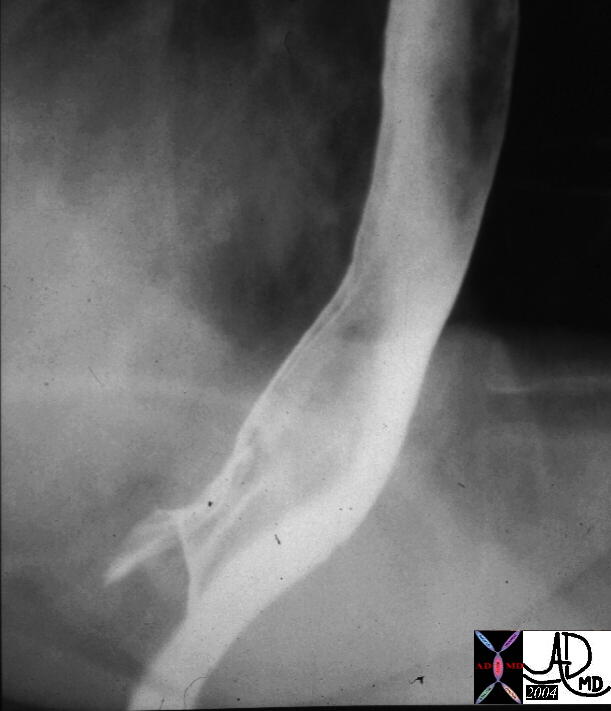
The double contrast barium swallow shows the esophagus as a distended featureless tubular structure with smooth mucosa. This appearance is an artificial appearance of the esophagus since it is as a result of reflux of air from the stomach and inhibition of the primary stripping wave induced by the method of the study.
Courtesy of: Ashley Davidoff, M.D. 49741
The thoracic esophagusuns from T1 to about T5. The esophagus is distended with air inthe double contrast study to optimise visualization of the mucosal surface, while the single contrast study enables evaluation of peristalsis.

The thoracic esophagus in this double contrast barium swallow on the left and single contrast study on the right runs from T1 to about T5. The esophagus is distended with air in the double contrast study to optimize visualization of the mucosal surface, while the single contrast study enables evaluation of peristalsis.
keywords esophagus GE junction gastroesophageal junction normal anatomy double contrast barium swallow upper GI
Ashley Davidoff MD TheCommonVein.net 39562b01
The thoracic portion courses to approximately the 5th thoracic vertebrae. The thoracic portion can itself be subdivided into the upper, middle, and lower regions.
The upper region runs from the aortic arch superiorly while the middle region courses from the aortic arch to the inferior pulmonary vein.
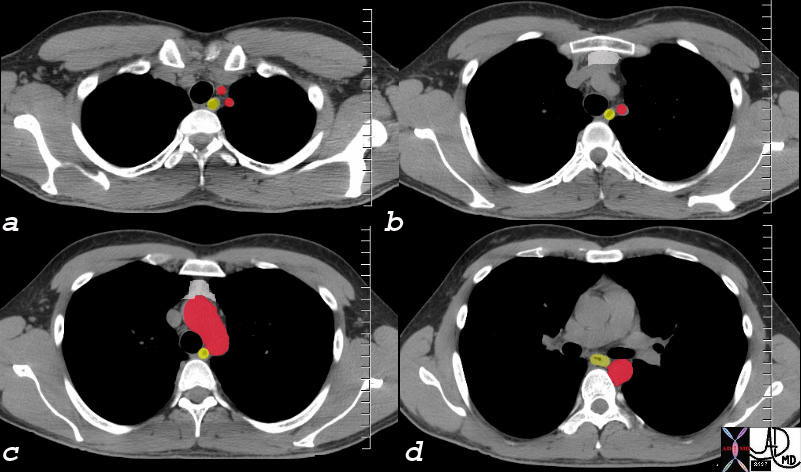
The CT scan of the upper chest shows the esophagus (yellow) at the thoracic inlet (a) leftward of the trachea (black) and medial to the left subclavian artery (a and b). Lower down the trachea remains medial while the aortic arch becomes an anterior and lateral relation.(c) Below the carina, (d) the left main stem bronchus is an anterior and leftward relation while the descending aorta lies lateral.
key words: esophagus relations left subclavian artery trachea aortic arch ;left main stem bronchus normal thymus 30 year old normal anatomy CTscan C
Ashley Davidoff MD TheCommonVein.net 73610c02
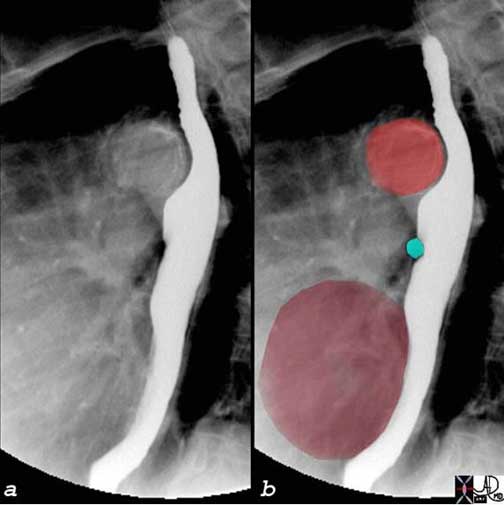
The normal indentations on the esophagus include the aortic arch and knob seen in bright red in b. The left bronchus is usually seen as a oblique line crossing the back of the esophagus, but in this case is seen as a focal indentation on the anterior wall. The left atrium is seen pulsating against the distal esophagus (maroon) usually when the left atrium is enlarged.
Ashley Davidoff, M.D. TheCommonVein.net
Finally, the abdominal portion runs from the inferior pulmonary vein to the LES or GE junction.
There is an overall slight S shape to the esophagus as it descends. There is a convexity towards the left at the upper esophagus and a “right turn” at the lower esophagus around the 7th thoracic vertebrae.
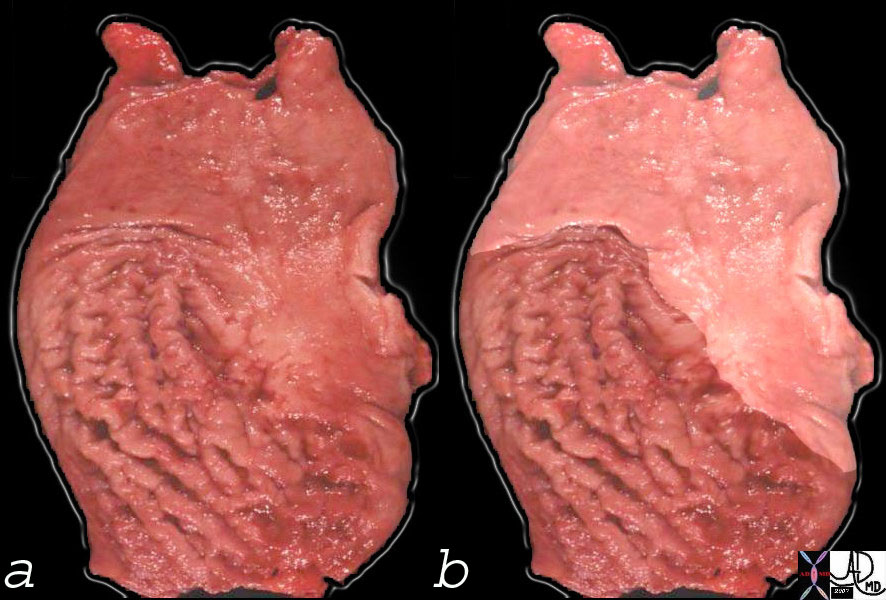
Gross anatomy on the left of the Z line of the GE junction. On the right the squamous mucosa has been accentuated
Keywords esophagus stomach GE junction gastroesophageal junction mucosal folds rugae anatomy grosspathology normal
Ashley Davidoff, M.D. TheCommonVein.net 00633c01
 GE junction GE junction |
| keywords esophagus GE junction normal contrast barium X-Ray UGI upper GI imaging radiology Ashley Davidoff MD TheCommonVein.net 00300 |


Ashley Davidoff TheCommonVein.net esophagus-0002
The gastroesophageal junction (aka Z line, ZZ line or squamo-colunar junction) is clearly outlined as the squamous epithelium (white) transitions to the gastric epithelium (reddish pink mucosa)
Ashley Davidoff MD TheCommonVein.net 73474
Applied Biology
There are many conditions that can affect the subdivisions of the esophagus. Neurologic conditions can alter the normal propagation and functioning of the esophagus. Systemic conditions, such as Scleroderma or Systemic Lupus Erythematosus, can also greatly affect proper esophageal function. Whether the dysfunction is secondary to smooth or skeletal muscle involvement, or vascular or neurologic impairment, the physiologic sequela can be quite significant.
keywords esophagus web Pattison Kelly Plummer Vinson squamous mucosa proliferation mechanical obstruction dysphagia barium swallow imaging radiology
Ashley Davidoff MD TheCommonVein.net 01184c03
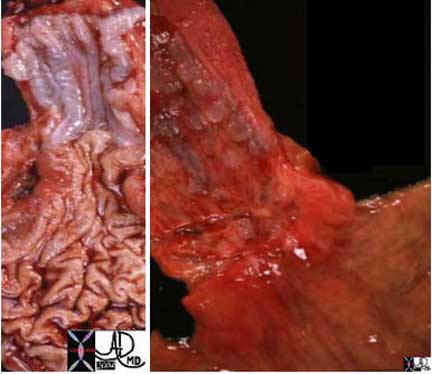
The GE junction is a distinct border as seen normally in the left image. The distal esophagus is normally a pearl white hue, while the gastric mucosa is a pink hue. In esophagitis the hyperemic inflammatory changes make the border less distinct (right image).
Ashley Davidoff, M.D. TheCommonVein.net
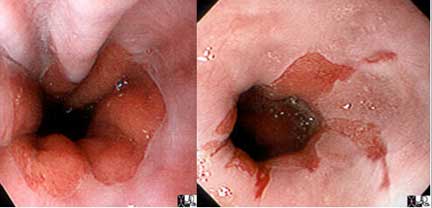
The extension of the gastric mucosa as “cracks” in the otherwise pearly white esophageal mucosa represents metaplasia (a growth and character change) of the normal squamous mucosa into gastric mucosa.
Courtesy of: Joshua Namias, M.D. and Ashley Davidoff, M.D. TheCommonVein.net
There is no capsule and the esophagus is attached to the other mediastinal structures by loose connective tissue.

Keywords esophagus pedunculated polyp inflammatory polyp GE junction gastroesophageal junction barium swallow Ashley Davidoff, M.D. TheCommonVein.net 01191
At the GE junction the distal esophagus and GE junction is connected to the liver by the gastrohepatic ligament at the fissure for the ligamentum venosum., and attached to the diaphragm by the phrenico-esophageal ligament. It is the latter ligament that gets stretched in the aging process resulting in loss of GE junction anchorage and the evolution of hiatal hernias in the aging process.