The Common Vein Copyright 2007
Joshua Namias MD
Ashley Davidoff MD
Definition
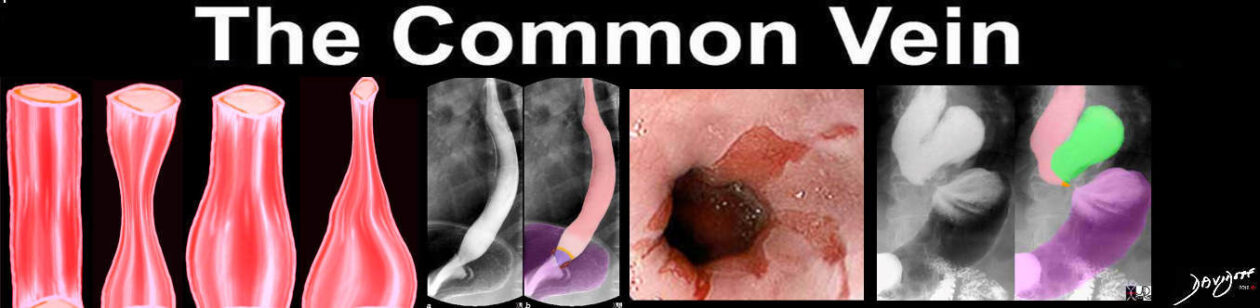
Endoscopy of the esophagus is a procedure that enables diagnostic evaluation and often treatment of esophageal diseases.
The endoscope is a flexible fiberoptic camera that can be placed into the mouth or anus for real-time visualization of the Gastrointestinal tract. Derived for the Greek words “endo” (within) and scope (view), the first reference to this modality was by Hippocrates in regards to an anal evaluation.
The more modern scope was prototyped by Basil Hirshowitz in 1958 and the more advanced scopes used today we built on his advances.
Indications
Endosocopy has an important role in diagnosing esophageal disorders, in addition to those of the upper intestinal tract. Typically endoscopic studies are performed when there is concern for a luminal irregularity such as esophagitis, Barrett’s Esophagus (in the setting of long standing GERD), rings/strictures, and malignancy.
Endoscopic ultrasound is especially useful in delineating the extent (depth) of esophageal mucosal lesions such as cancer.
It is important to realize that endoscopic studies are often used in conjunction with many other tests to be described below.
Contraindications
When done in the appropriate clinical setting, endoscopy is a safe and helpful diagnostic tool. However, it is an invasive procedure and with it comes possible complications. To avoid complications, the endoscopist must be able to identify those patients in whom endoscopy could cause more harm than benefit from the procedure.
As such, contraindications for endscopy include patients whose hemodynamic status prevents safe administration of the required sedatives. The sedatives and narcotics given can cause a drop in blood pressure in addition to suppressing respiration.
To properly perform endoscopy, the lumen must be insufflated with air. If a patient has concern for, or has a documented, perforated viscus, air insufflation would worsen the condition. Referring to LaPlace’s law, the diameter of the lumen would increase thus increasing surface tension and the risk of perforation
Advantages
The advantage of endoscopy is that the pathology can be biopsied through the scope. The scope has several channels that allow objects to be passed into the organ being evaluated. The biopsy forceps can be directed directly to the abnormal tissue and the tissue removed for histopathologic evaluation.
Therapeutic intervention can also be performed through the endoscope. As described above, treatment of Barrett’s esophagus can be accomplished with the endoscope. Treatment modalities include APC, photodynamic therapy, mucosal resection, amongst others.
Dilation of strictures or rings can be accomplished with balloons passed through the endoscope. This allows for visualization of the mechanical disruption with these devices.
Retrieval of foreign bodies is a common therapeutic intervention performed with the endoscope. Patients who present with food bolus that can’t pass on their own are often scoped with the goal of removing the bolus. Patients who ingest objects, while intentionally or unintentionally, that get stuck in the esophagus can have them removed. Again, through the scope, baskets, snares, nets, can all be passed to retrieve the objects.
Endoscopic Ultrasound is a relatively new modality that encorporates traditional endoscopy and the properties of ultrasonography. A special ultrasound is fitted onto the distal end of the scope and thus provides excellent visualization of the layers of the esophagus and the surrounding structures. Biopsies can also be taken of the identified pathology including the esophagus proper, masses, lymph nodes and other masses near the esophagus.
Disadvantages
The main disadvantage to endscopy is that it is a invasive procedure that requires sedation. While typically thought of as a relatively benign invasive test, complications can quickly arise.
Patients need to be hemodynamically stable and able to withstand the anesthesia and the stress of the procedure itself.
Aim
The upper endoscope has multiple important uses in regards to evaluating, diagnosis, and treating esophageal pathology. This modality allows the Gastrointerologist to visualize the esophageal mucosa and lumen. Evidence of inflammation, ulcers, strictures, and masses all can therefore be appreciated.
Patient Preparation
For upper endoscopy the patient is kept in the fasting state for at least 4-6 hours. The main reason this is required is to reduce the risk of aspiration with the anesthesia. Visualization is often impaired with upper endoscopy if food is present
in the stomach.
The ideal colonoscopic preparation has the patient consume a clear liquid diet the day prior to the procedure. Starting the afternoon before the procedure, the patient takes an oral cathartic. There are many different types of preparations in the market today.
The day of the procedure, the patient presents in the fasting state.
Ideally, patients should be off of all anticoagulation and platelet inhibitors. Most standardized preparations ask the patient to hold all aspirin and NSAIDs for approximately one week so as to avoid increased risk of bleeding.
Equipment
Each procedure room is equipment with patient monitoring systems that allows for continues measurements of blood pressure, heart rate, respiratory rate, and oxygen saturation. A TV screen is located across from the endoscopist with the scope processor capturing images. One to two nurses are present to assist with sedation, patient monitoring, and therapeutic interventions. Each room typically has all the equipment that may be needed during cases such as biopsy forceps, snares, clips, baskets and the like.
Procedure/Technique
Patients are typically brought into the procedure room and placed in the left lateral decubitus position. An IV is placed so sedative medications can be given intraveniously. When performing an endoscopy, once the patient is sedated the endoscope is placed into the mouth. Visualization of the tongue and posterior oropharynx allows for passage into the esophagus. The scope is then carefully passed through the esophagus into the stomach and small intestine.
Similarly, for colonoscopy, once the patient is comfortable, the flexible scope is passed into the anus and rectum to allow for real-time visualization of the entire colonic mucosa.
Images are displayed on television sets which are often located on both sides of the room.
Once the test is completed, the patient is brought to the recovery area where they rest for approximately one hour while the medications wear off. The patients are discharged to home with an escort and instructed not to drive, drink alcohol, or perform manual labor for the remainder of the day.
Complications
The overall risk of complications during endscopic procedures is quite low, especially in the hands of a experienced endoscopist. In addition to the risk of received conscious sedation (allergic reaction to sedatives, respiratory compromise, hemodynamic changes), the risks of the procedure itself include aspiration, bleeding, perforation.
Aspiration is higher in patients undergoing upper endoscopy given the passage of the camera through the mouth.
Bleeding can occur for various reasons. Trauma from the passage of the scope can occur, although is quite rare. Bleeding can occur when diagnostic or therapeutic interventions are performed. With biopsy of the mucosa, local bleeding can occur, but typically are self-limiting. A common scenario seen by the endoscopist is of a patient who has a polyp removed at colonoscopy and who restarts their aspirin earlier that the recommended time (typically 1-2 weeks). The anti-platelet function of the aspirin results in bleeding from the polypectomy site.
Perforation is a rare, but often serious complication of both upper and lower endoscopic procedures. In experienced hands, the perforation rate of colonscopy is thought to be approximately 1/1000 for a diagnostic colonoscopy.
Conclusion
Endoscopy is an exteremely useful and safe diagnostic as well as a therapeutic tool . It is also provides a life saving measure in certain conditions.